5. Treatment of Adrenal Insufficiency
SUSPECTING AN ADRENAL CRISIS?If a person presents in an adrenal crisis (a potentially life-threatening condition), treatment should not be delayed while waiting for test results! Click here for step-by-step instructions.
In the majority of cases, adrenal insufficiency is a chronic and irreversible condition that requires life-long hormone replacement therapy. There is no cure available.
Treatment requires the replacement or substitution of the hormones that the adrenal glands ceased to produce and should begin as soon as the diagnosis is confirmed.
5.1. Cortisol replacement
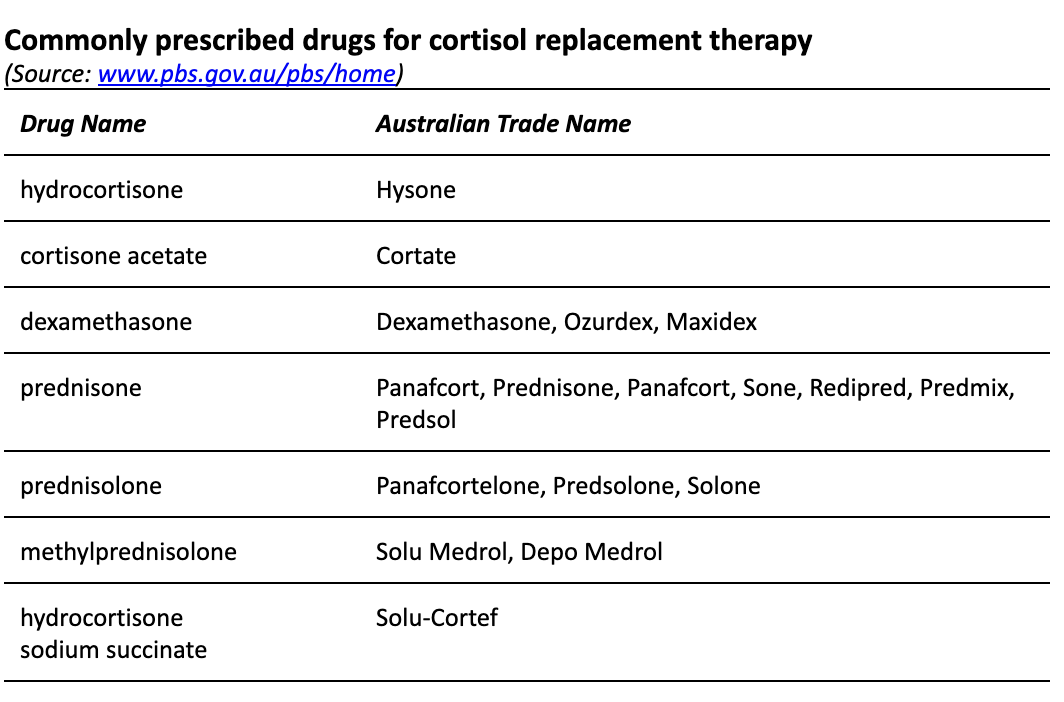
The preferred treatment of adrenal insufficiency is oral hydrocortisone which is the most physiological option for cortisol replacement available today. The patient’s well being usually dramatically improves within 24 hours after the first dose is taken.
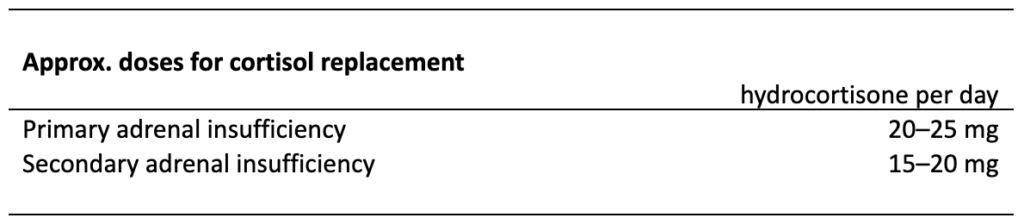
Table 4: Cortisol replacement – Note that dosing amounts vary depending on patient profile
The daily hydrocortisone dose should be given in two to three doses, with half to two thirds of the total daily dose in the morning. The goal should be to mimic the circadian rhythm of the physiological cortisol production as closely as possible.
Since every person with adrenal insufficiency has a different residual function of their adrenal glands and a different metabolism, fixed dosage recommendations are not available. Dosing needs to be adjusted to meet the needs of each individual. It is highly recommended to have an endocrinologist oversee and manage dosage and necessary adjustments.
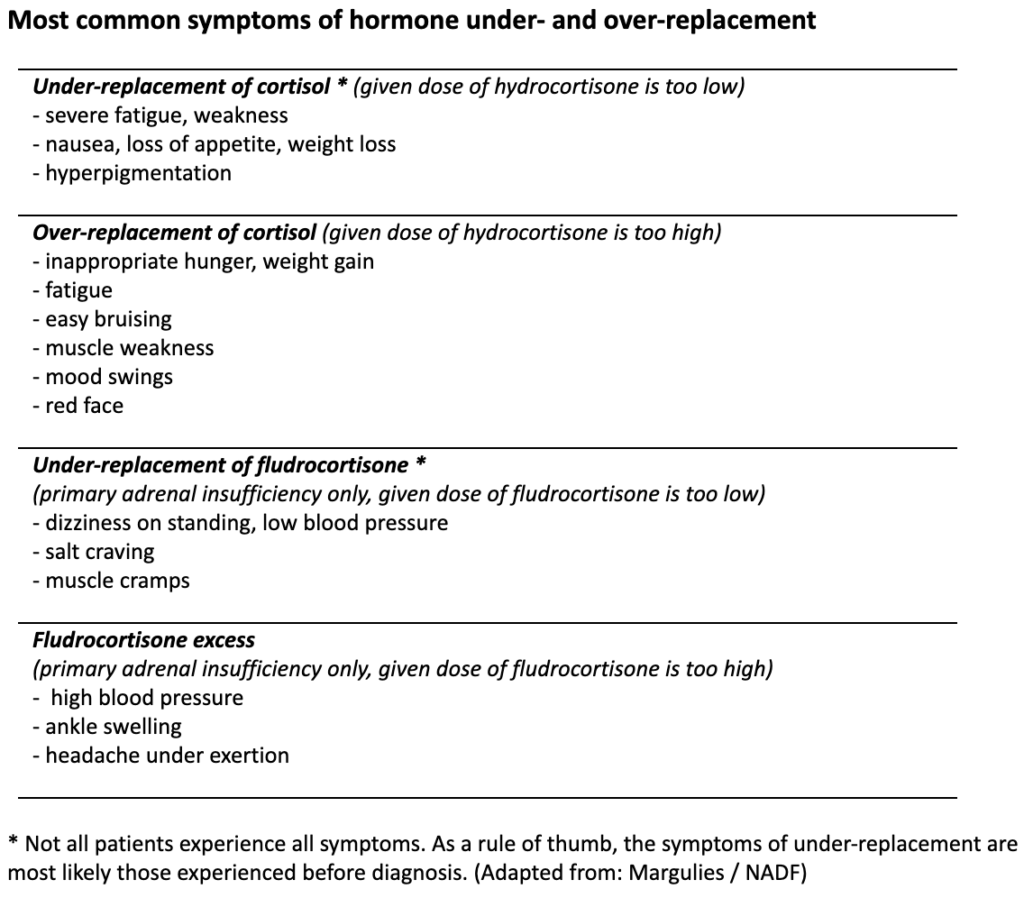
Unfortunately, there are no reliable or “easy tests” to assess how effective the replacement therapy is. Some clinicians prefer to use cortisol day curves for treatment monitoring and dose titration whereas others rely on the clinical symptoms reported by their patients to adjust and optimise dosing.
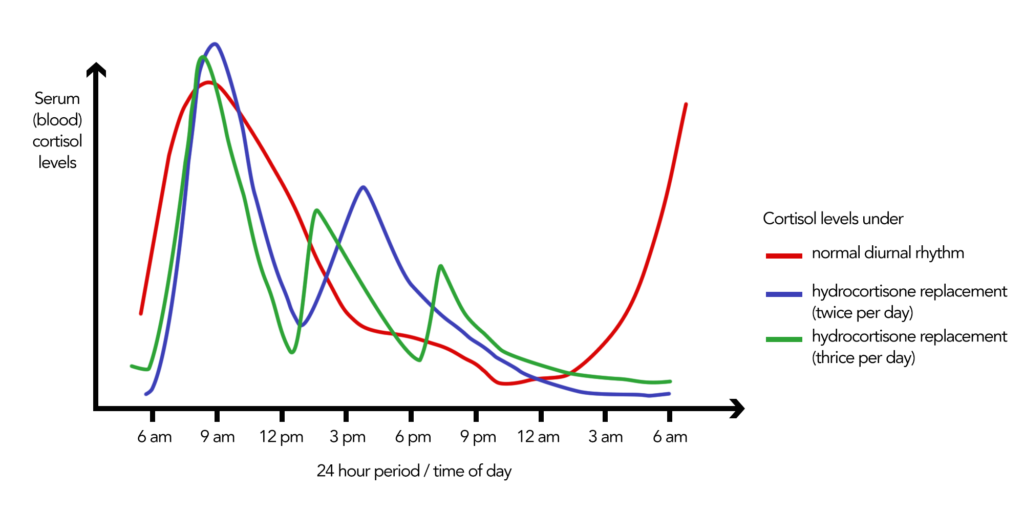
Figure 7: Comparison of physiological cortisol levels in healthy people and levels reached under hydrocortisone replacement
Outlook – Novel treatment options under development
Research has shown that it is possible to better mimic the physiological circadian rhythm of cortisol with special “modified-release” hydrocortisone preparations. A number of drugs are currently under clinical investigation and a few have recently been introduced in some European countries:
Plenadren is a once-daily dual-release hydrocortisone tablet taken in the morning. It contains a rapid-release coating and a timed-released inner core of hydrocortisone. Plenadren currently enjoys orphan status as a licensed treatment for adrenal insufficiency by the European Medicines Agency (EMA).
Chronocort offers a delayed and sustained release of the hormone. When taken at bedtime, it maintains low cortisol levels during midnight with an early morning peak. Its manufacturer Diurnal is committed to conduct more clinical studies in the US in the future.
Future studies will show whether these new preparations stand up to the promise of improving cardiovascular risk factors, glucose metabolism and quality of life. Neither one is currently available in Australia.
Not all people respond well to oral hydrocortisone
Some people metabolise oral hydrocortisone very quickly and require a more continuous hydrocortisone supply that mimics the normal circadian cortisol rhythm. This can be achieved, for instance, by using a subcutaneous infusion or “pump”, similar to insulin pumps used by diabetic patients. So far, pumps are rarely used in patients with adrenal insufficiency but can be a good option for people who are doing poorly on oral steroids.
“I am now on a pump because I rapidly metabolise oral medication, and my adrenal insufficiency has much improved since commencing the pump.” – Desley
The difference between replacement therapy and steroid treatment of other conditions
It is important to understand that there is a difference between replacing a hormone that is no longer produced by the body and taking high(er) doses of cortisone to treat another condition such as asthma. The feared side effects associated with cortisone treatment such as osteoporosis, weight gain, glaucoma, or mood changes are not to be expected when replacing cortisol in adrenal insufficiency.
5.2. Aldosterone replacement
In primary adrenal insufficiency mineralocorticoid (aldosterone) replacement therapy is necessary to stabilise blood pressure (prevent sodium loss, intravascular volume depletion and hyperkalaemia).
Aldosterone is given in the form of fludrocortisone (fludrocortisone acetate, Florinef) in a dose of 0.05–0.20 mg daily, taken in the morning. The dose may have to be increased in the summer under medical supervision, especially if temperatures are high.
Signs of mineralocorticoid under-replacement are a drop in blood pressure after standing up, weight loss, and dehydration (blood test: plasma renin level increased, hyponatraemia). Signs of an over-replacement are weight gain and increased blood pressure (blood test: hypernatraemia, suppressed plasma renin activity).
GOOD TO KNOWAldosterone replacement is not needed if the daily hydrocortisone dose exceeds 50 mg.
People living with secondary or tertiary adrenal insufficiency usually (but not always!) produce enough aldosterone and therefore don’t require aldosterone replacement.
5.3. Androgen replacement
In women, the adrenal cortex is the main source of androgen production.
Treatment with dehydroepiandrosterone (DHEA) may improve mood and general wellbeing and may be considered in people whose wellbeing is greatly impaired despite optimal glucocorticoid and mineralocorticoid replacement. Discuss this with your endocrinologist.
For people living with adrenal insufficiency, it is important to understand that:
– Hormone replacement is essential for life.
– Tablets need to be taken every day, at the right and same time of day. They may be taken on an empty stomach.
– Never abruptly stop taking your medication.
– Always carry extra medication and an emergency kit containing Solu-Cortef, syringes and needles.
– Dosage requirements may change over time.
> NEXT CHAPTER
> CHAPTER OVERVIEW
Anatomy/Physiology | Types of Adrenal Insufficiency | Symptoms | Testing/Diagnosis | Treatment | Stress dosing/Sick day Management | Adrenal Crisis | Quality of Life and Risks | Other Conditions and Drugs | Long-term Management | Suggested Reading | Literature/References
Author: Gisela Spallek, MD PhD
Edited by Maria Stewart, Director of AIC and deputy editor Des Rolph, Associate Director of AIC

