1. Anatomy and Physiology
1.1. The Adrenal Glands
The adrenal glands (also called suprarenal glands) are situated on top of each kidney. They are small but powerful and look like two little upside down acorns. They secrete steroid and catecholamine hormones directly into the blood.
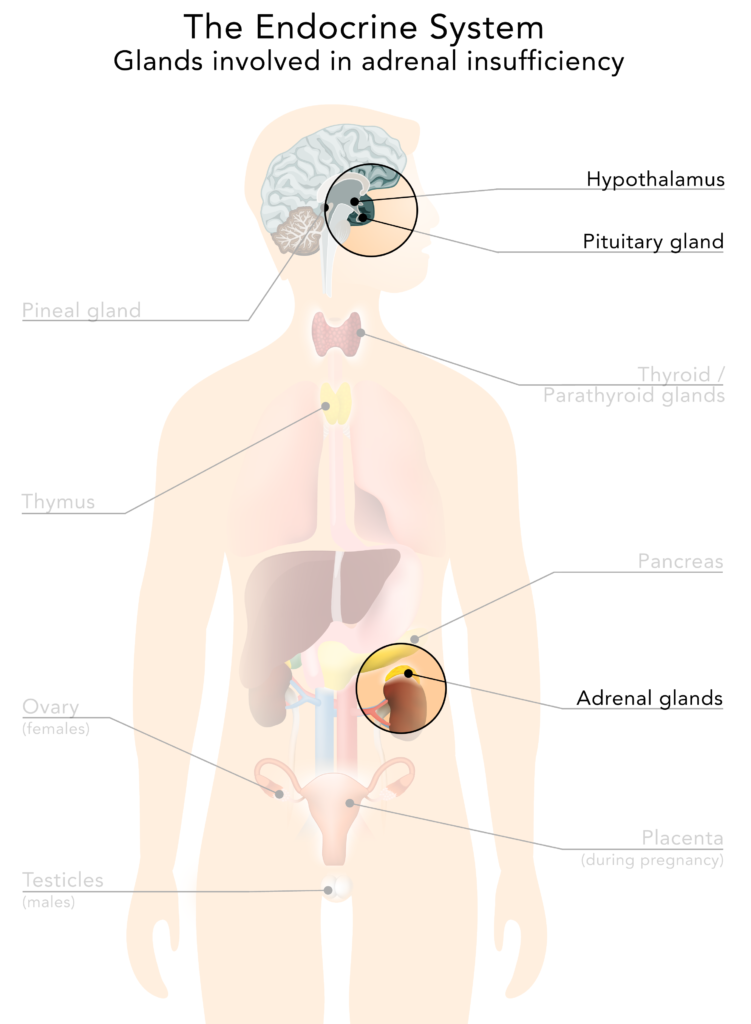
Figure 1: The endocrine system, with a focus on adrenal insufficency
Each adrenal gland has an outer cortex which produces steroid hormones and an inner medulla. The adrenal cortex itself is divided into three zones: zona glomerulosa, zona fasciculata and zona reticularis which produce the three main types of steroid hormones: mineralocorticoids, glucocorticoids and androgens.
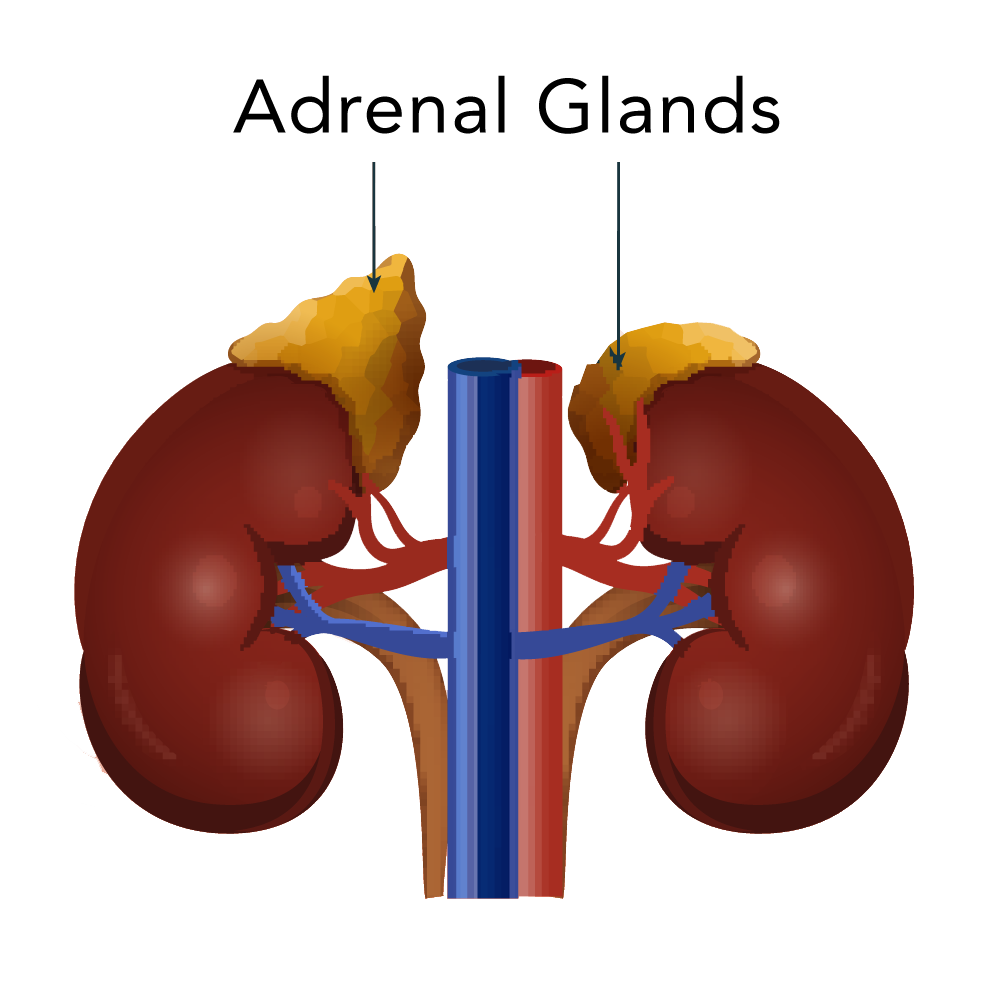
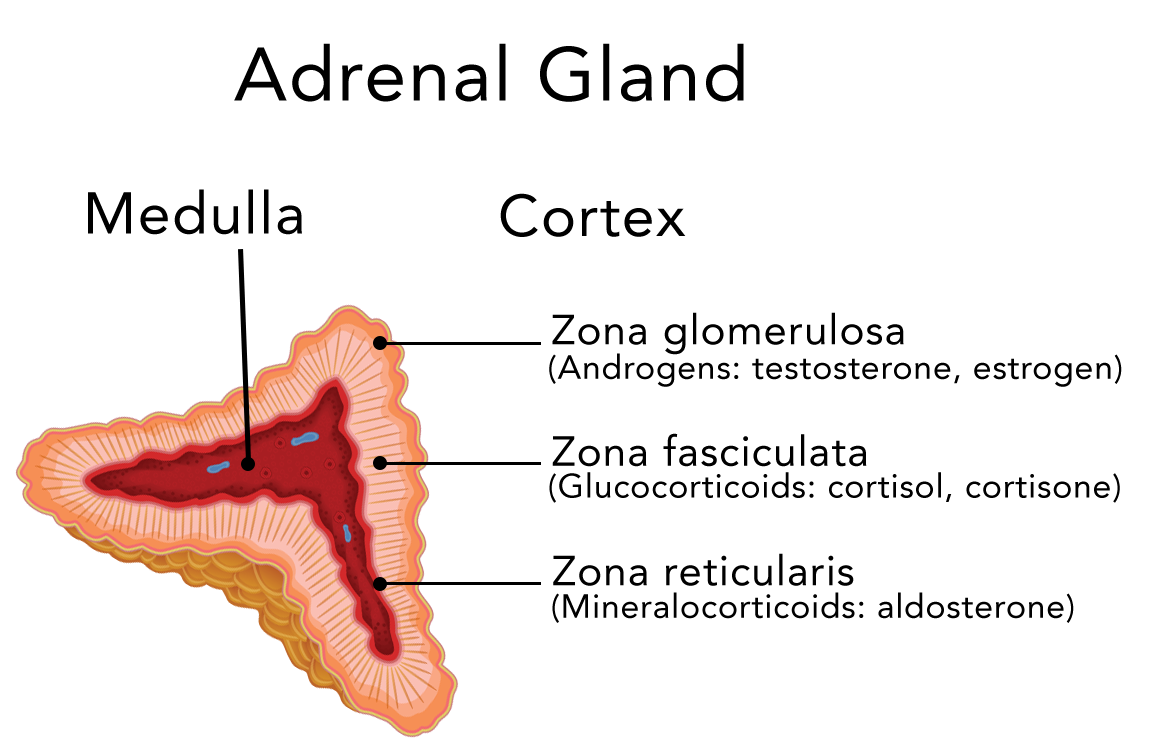
Figure 2a: Anatomical sketch of the adrenal glands
Figure 2b: Histological sketch of the layers of the adrenal glands and hormones they produce
1.2. What is Cortisol?
Cortisol is a steroid hormone, also known as glucocorticoid, and is produced in the cortex of the adrenal glands. Cortisol is released into the blood and transported all around the body. Almost every cell contains receptors for cortisol, and the cell type determines what affect the cortisol has.
These effects, among many others, include:
- controlling the body’s blood sugar levels and thus regulating metabolism;
- acting as an anti-inflammatory;
- influencing memory formation;
- regulating blood pressure.
The regulation of Cortisol Release: The Hypothalamic-Pituitary-Adrenal (HPA) Axis
The secretion of cortisol is mainly controlled by three inter-communicating regions of the body: the hypothalamus, the pituitary gland (both in the brain) and the adrenal gland (see above, figure 1). Together they form our central stress response system and are commonly referred to as the hypothalamic-pituitary-adrenal axis (HPA axis).
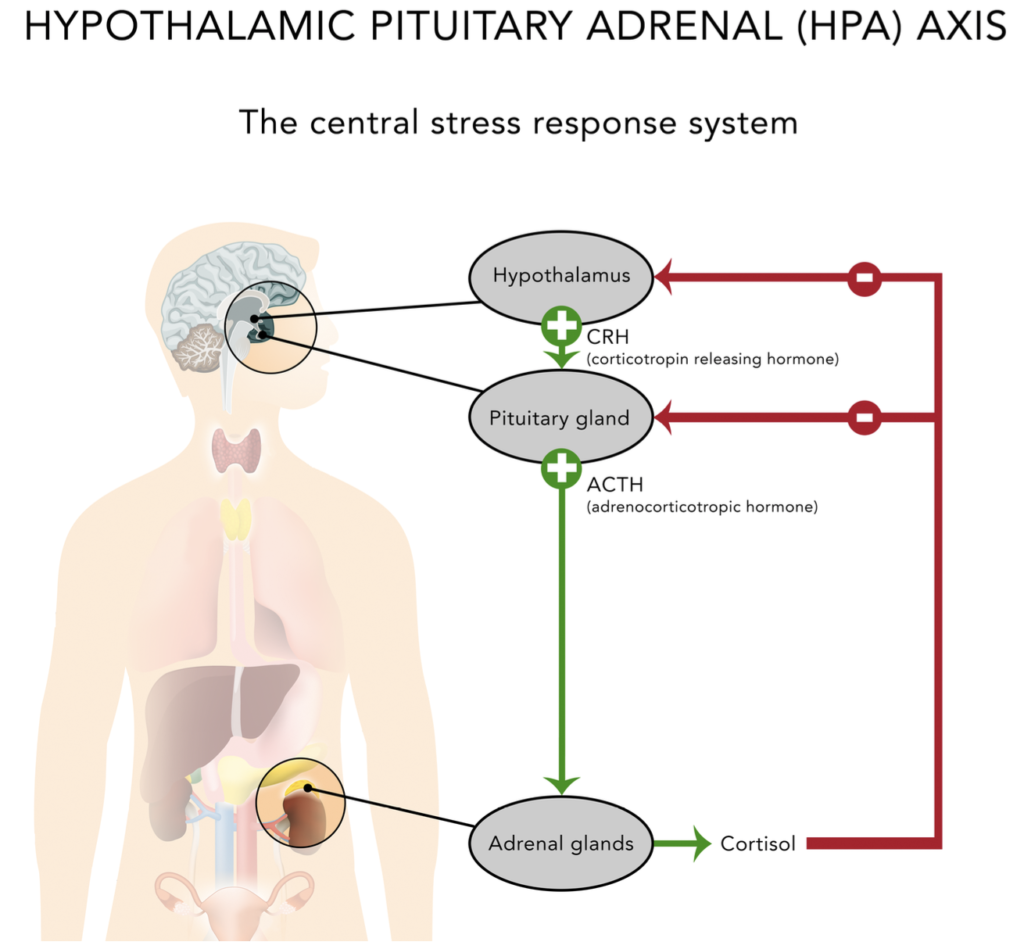
Figure 3: HPA (hypothalamic-pituitary-adrenal) Axis
Normally, when blood cortisol levels are low, a group of cells in a region of the brain called the hypothalamus releases corticotropin releasing hormone (CRH) which then causes the pituitary gland to secrete the hormone ACTH (adrenocorticotropic hormone, also called corticotropin, adrenocorticotrophin) into the bloodstream.
High blood levels of ACTH are detected in the adrenal glands and stimulate the secretion of cortisol, causing blood levels of cortisol to rise. As the cortisol levels rise they start to block the release of (more) CRH from the hypothalamus and ACTH from the pituitary gland. As a result ACTH blood levels start to drop which then leads to a drop in cortisol levels. This is called a negative feedback loop.
Circadian Rhythm of Cortisol Release
The hypothalamus also acts as the body’s “central clock”. In healthy people the production of cortisol follows a daily rhythm, with the highest peak around wake-up time and two smaller peaks around noon and late afternoon. The blood levels are lowest in the evening and early part of the night. In addition, extra cortisol is released in response to stress to help the body to cope and respond appropriately.
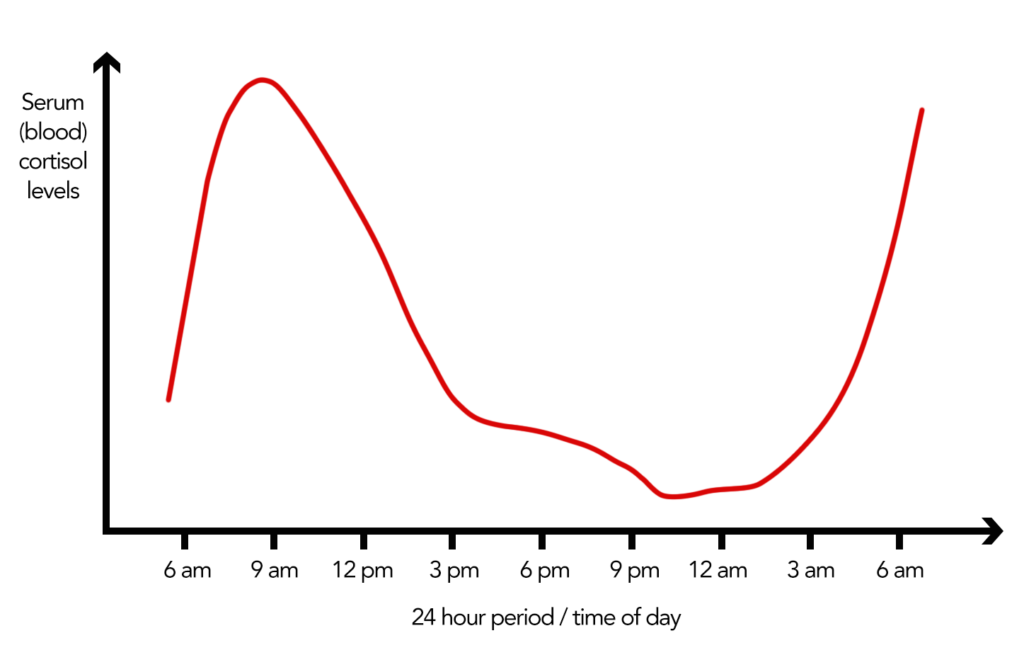
Figure 4: Physiological blood cortisol levels over the period of 24 hrs.
GOOD TO KNOWSoon after waking in the morning, cortisol blood levels rise to the highest levels of the day. People living with adrenal insufficiency usually have low levels of morning cortisol, and getting out of bed can be difficult. They should take their first hydrocortisone dose right after waking up, or even half an hour before getting out of bed.
One of the challenges in the treatment of adrenal insufficiency is to mimic the normal rhythm of cortisol release as closely as possible. So far, conventional oral medication (tablets/pills taken by mouth) such as immediate-release hydrocortisone is not capable of fully replicating the physiological cortisol circadian rhythm, even when given twice or thrice daily.
Interesting fact: In people who work at night the cortisol release pattern is reversed, which shows that the release of cortisol is linked to daily activity patterns.
1.3. What is Aldosterone?
Aldosterone, a mineralocorticoid, helps maintain the blood pressure in the body by helping the kidneys retain sodium and excrete potassium. When aldosterone production falls too low, the kidneys are not able to regulate the salt and water balance, causing blood volume and blood pressure to drop.
Whereas all adrenal insufficient people need cortisol replacement, those with secondary and tertiary adrenal insufficiency usually still produce aldosterone and androgens. Therefore, typically only people living with primary adrenal insufficiency need to replace those hormones as well.
> NEXT CHAPTER
> CHAPTER OVERVIEW
Anatomy/Physiology | Types of Adrenal Insufficiency | Symptoms | Testing/Diagnosis | Treatment | Stress dosing/Sick day Management | Adrenal Crisis | Quality of Life and Risks | Other Conditions and Drugs | Long-term Management | Suggested Reading | Literature/References
Author: Gisela Spallek, MD PhD; graphics by spallek.com
Edited by Maria Stewart, Director of AIC and deputy editor Des Rolph, Associate Director of AIC

